What you need to know as a GP
Lung cancer is the leading cause of cancer death in Australia, often diagnosed late, with a 5-year survival rate of just 18%. The death rates of lung cancer outnumber the deaths caused by breast, colon, and prostate cancer combined.
The new National Lung Cancer Screening Program is a major step forward-offering low-dose CT scans to high-risk individuals to detect lung cancer earlier and save lives.
But success depends on more than policy. It relies on GPs who identify risk, start conversations, and guide patients through screening. Your role is critical in educating, referring, and supporting patients, helping reduce mortality through early detection.
This isn’t just screening-it’s a chance to make a real difference.
=================================================================================================================
Who is eligible?
The program will target people aged 50 to 70 years who are current or former smokers (within the last 10 years) with a 30 pack-year smoking history.
How does it work?
Eligible individuals identified by their GP will be invited to undergo a BULK BILLED low-dose CT (LDCT) screening every two years. This approach aims to detect cancer at earlier, more treatable stages-when patients are asymptomatic. The referral process will center around GP-led assessments and shared decision-making conversations.
Where and when?
The program will begin in July 2025. This is a pivotal opportunity to reshape outcomes in Australia’s deadliest cancer. Staying informed and prepared will help ensure your patients
are among the first to benefit. Lung cancer is a silent killer. Low-dose CT screening improves early detection and cure.
A quieter revolution in lung cancer care:
1. Research shows the program could reduce lung cancer deaths by up to 24% in high-risk groups significant impact.
2. Early detection often means the difference between a cure and palliative care.
3. Screening greatly increases the chances of finding cancer at Stage I or II, allowing for more effective treatments like surgery or targeted therapy.
4. More early diagnoses lead to fewer emergency cases, easing pressure on hospitals and emergency departments.
5. Most importantly, patients and families gain a better quality of life-less time in treatment, more time together. Increased workload on Respiratory Clinics
• We understand from Australian research on the lung cancer screening program that 1-5% of CT chest scans will discover a lung cancer.
• We also know that many CT scans (around 90%) will have non-cancer-related abnormalities that require assessment.
• We expect a high number of referrals for Respiratory Clinics and have already implemented clinic availability for this work, as a result of the lung cancer screening
program.
Additional lung cancer/lung nodule clinics at Sydney Respiratory Specialist
We have a dedicated space to assess node/cancer referrals starting from 1st July 2025.
Dates: Tuesdays and Fridays
Times: 8 am-4 pm
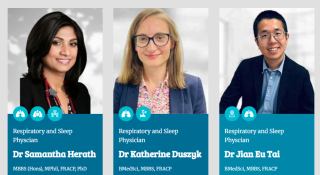
Respiratory specialists: Dr Samantha Herath and Dr KV Singh
• Time Frame: We will see patients within 48 hours of referral and organise appropriate assessments. If lung cancer is suspected, we will perform all required bronchoscopic biopsies for diagnosis and refer for treatment within 2 weeks.
• Dr Singh and Dr Herath are skilled EBUS proceduralists. Therefore, the patient does not need to see another specialist for these procedures-saving time and money and streamlining the process for the patients.
• (National guidelines suggest a time frame of 2 weeks to see a specialist from the time of GP referral and 6 weeks to commencement of treatment. At Sydney Respiratory Specialist Clinic, we pride ourselves on achieving a much faster turnaround time.) Clinical guidelines and checklists for GPs:
• Access the National Lung Cancer Screening Program Clinical Guide and GP referral checklist directly from the Department of Health portal:
Clinical guidelines and checklists for GPs:
Access the National Lung Cancer Screening Program Clinical Guide and GP referral checklist directly from the Department of Health portal:
Patient communication tools:
• Printed brochures, digital explainers, and culturally safe materials are available to help you guide discussions with patients-especially those who may be hesitant or
unfamiliar with the concept of lung screening.
https://www.lungcancerresearchfoundation.org/for-patients/print-and-digital-resources/

Let’s keep this dialogue open
We know that implementing a national screening program will come with questions, complexities, and curved paths. You don’t have to navigate them alone. If you’d like to discuss a case, clarify the referral process, or share feedback, we welcome your input.
Reach us at info@sydneyrespiratory.com.au or call our clinic on 02 9487 3473, or contact our practice manager, Kelly, on 0457 262 886, if you wish to speak to
one of our respiratory specialists directly. Suite 18, level 1, Parkway SAN Clinic, 172, Fox Valley Road, Wahroonga, NSW 2076